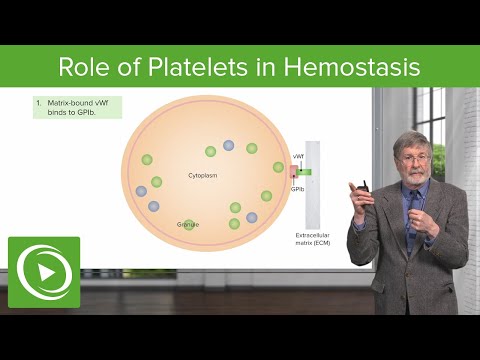
Platelets contribute their hemostatic capacity via adhesion, activation and aggregation, which are triggered upon tissue injury, and these actions stimulate the coagulation factors and other mediators to achieve hemostasis.
Q. What activates platelets during hemostasis?
Platelets contain secretory granules. When they stick to the proteins in the vessel walls, they degranulate, thus releasing their products, which include ADP (adenosine diphosphate), serotonin, and thromboxane A2 (which activates other platelets).
Table of Contents
- Q. What activates platelets during hemostasis?
- Q. What happens to platelets when they become activated?
- Q. Which of the following factors are released from activated platelets?
- Q. What are the 4 steps of hemostasis?
- Q. What are the 5 stages of hemostasis?
- Q. What are five factors that affect hemostasis?
- Q. What are the two major disorders of hemostasis?
- Q. How is hemostasis maintained?
- Q. What happens during primary hemostasis?
- Q. What is normal hemostasis?
- Q. What is adequate hemostasis?
- Q. What is needed for hemostasis?
- Q. What are the two forms of hemostatic agents?
- Q. When would you use clotting powder?
- Q. What is hemostatic dressing made of?
- Q. What are hemostatic agents made of?
- Q. Does Celox hurt?
- Q. What is the best hemostatic agent?
- Q. Is QuikClot safe to use?
- Q. How long is QuikClot good for?
- Q. Can you use QuikClot on abdomen?
- Q. How long should packing stay in wound?
- Q. When should a wound be packed?
- Q. Do you pack a bullet wound?
- Q. Is it better if a bullet goes through you?
- Q. What wounds can you pack?
- Q. Does sugar help wounds heal faster?
Q. What happens to platelets when they become activated?
Activated during this process, platelets change shape and release the contents of their granules. Active GP IIb/IIIa receptor has central role in mediating platelet aggregation. Platelet activation is stimulated by bound platelet secretion products and local prothrombotic factors such as tissue factor.
Q. Which of the following factors are released from activated platelets?
During platelet activation, the platelet releases a number of important cytokines and chemical mediators via degranulation. The released chemicals include ADP, VWF, thromboxane A2, platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), serotonin, and coagulation factors.
Q. What are the 4 steps of hemostasis?
The mechanism of hemostasis can divide into four stages. 1) Constriction of the blood vessel. 2) Formation of a temporary “platelet plug.” 3) Activation of the coagulation cascade. 4) Formation of “fibrin plug” or the final clot.
Q. What are the 5 stages of hemostasis?
Terms in this set (16)
- Vessel Spasm.
- Formation of Platelet Plug.
- Blood Coagulation.
- Clot Retraction.
- Clot Dissolution (Lysis)
Q. What are five factors that affect hemostasis?
It is affected by the characteristics of blood vessel walls, platelets, the fibrinolytic system, and the coagulation pathway, which are all intimately related ( Figure 1). All these factors function normally to produce an equilibrium between antithrombotic and prothrombotic factors.
Q. What are the two major disorders of hemostasis?
The most common inherited diseases are von Willebrand disease (primary hemostasis), which is the most common inherited disorder of hemostasis, and hemophilia A (factor VIII deficiency, secondary hemostasis).
Q. How is hemostasis maintained?
Blood loss is stopped by formation of a hemostatic plug. The endothelium in blood vessels maintains an anticoagulant surface that serves to maintain blood in its fluid state, but if the blood vessel is damaged components of the subendothelial matrix are exposed to the blood.
Q. What happens during primary hemostasis?
Primary hemostasis occurs when platelets attach to a damaged or disrupted area of the endothelium. This adhesion allows the platelets to undergo a shape change and then aggregate together. Once adhered to each other a temporary platelet plug is created.
Q. What is normal hemostasis?
Hemostasis is the physiologic mechanism that stems bleeding after injury to the vasculature. Normal hemostasis depends on both cellular components and soluble plasma proteins. Circulating platelets adhere and aggregate at sites of blood vessel injury.
Q. What is adequate hemostasis?
Hemostasis is the process of how the body stops bleeding from a cut or injury. In major trauma or surgery, physicians often need to help patients to achieve adequate hemostasis – in order to minimize blood loss and related injury.
Q. What is needed for hemostasis?
Hemostasis involves three basic steps: vascular spasm, the formation of a platelet plug, and coagulation, in which clotting factors promote the formation of a fibrin clot. Fibrinolysis is the process in which a clot is degraded in a healing vessel. They are important in limiting the extent and duration of clotting.
Q. What are the two forms of hemostatic agents?
Hemostatic agents come in two forms: granular powder and embedded/impregnated dressings.
Q. When would you use clotting powder?
Use WoundSeal Powder on external wounds that have blood, such as cuts, skin tears and avulsions. If sutures are required, the protective scab that forms may be removed by a medical professional by soaking it with saline solution and gently scraping it off.
Q. What is hemostatic dressing made of?
Hemostatic wound dressings It consists of a smectite mineral and a superabsorbent polyacrylic polymer that can absorb 200 times its own weight. An alternative approach to zeolite-based QuikClot®. which is based on alumino-phosphate chemistry, is currently under observation.
Q. What are hemostatic agents made of?
Fibrin sealants, gelatin-based products, oxidized cellulose, and collagen products are the major classes of topical hemostatic agents that have evolved over the last 100 years.
Q. Does Celox hurt?
It hurt like fire below the cut, I was scared that I might have nicked some tendon and I was almost positive that I had done some serious nerve damage to my favorite finger, but at least I knew I wasn’t going to bleed to death. Also, the Celox didn’t burn like the QuickClot they issued us in the USAF.
Q. What is the best hemostatic agent?
Hemostatic gauze dressings using the active ingredient chitosan include Celox, Chito-SAM and Hemcon. CoTCCC (the Committee on Tactical Combat Casualty Care) has long recommended QuikClot Combat Gauze as the hemostatic agent of choice for all branches of the US Military.
Q. Is QuikClot safe to use?
QuikClot® Gauze is impregnated with kaolin, a naturally occurring mineral proven to be effective as a hemostatic agent. Inorganic and inert, kaolin is non-allergenic, making it safe and effective to use. QuikClot® Gauze contains no botanicals and no animal or human proteins.
Q. How long is QuikClot good for?
Z-Medica(R), LLC, a leading developer and marketer of hemostatic devices, announces today that the sterility expiration date on its QuikClot Combat Gauze(R) products including QuikClot Combat Gauze, QuikClot Combat Gauze XL, QuikClot Combat Gauze TraumaPad, and QuikClot Combat Gauze LE is now five years.
Q. Can you use QuikClot on abdomen?
Intra-abdominal packing with laparotomy pads (LP) is a common and rapid method for hemorrhage control in critically injured patients. Combat Gauze™ and Trauma Pads™ ([QC] Z-Medica QuikClot®) are kaolin impregnated hemostatic agents, that in addition to LP, may improve hemorrhage control.
Q. How long should packing stay in wound?
Follow-up care If a gauze packing was put in your wound, it should be removed in 1 to 2 days. Check your wound every day for any signs that the infection is getting worse.
Q. When should a wound be packed?
When a wound is deep, or when it tunnels under the skin, packing the wound can help it heal. The packing material absorbs any drainage from the wound, which helps the tissues heal from the inside out. Without the packing, the wound might close at the top, without healing at the deeper areas of the wound.
Q. Do you pack a bullet wound?
Packing a Gunshot Wound. Gunshot wounds are incredibly deep and can cause severe internal bleeding. Applying external pressure often will not stop internal bleeding. Civilians will rarely have to do this but, if help is not coming anytime soon and the bleeding won’t stop, you can pack the wound.
Q. Is it better if a bullet goes through you?
The reason it is better is because a bullet that stays inside could cause lasting damage, like lead poisoning. Depends on what the bullet goes “straight through”. If it is your brain or heart, not so good. Through your shoulder, not good, but better.
Q. What wounds can you pack?
Wounds of the extremities and junctional areas are amenable to packing. If a tourniquet is initially placed on an extremity wound, it may later be replaced with a pressure dressing or with packing, which may be more comfortable for the patient and provide for a moderate amount of distal circulation.
Q. Does sugar help wounds heal faster?
To treat a wound with sugar, all you do, Murandu says, is pour the sugar on the wound and apply a bandage on top. The granules soak up any moisture that allows bacteria to thrive. Without the bacteria, the wound heals more quickly.