Carbon Monoxide: Hemoglobin binds carbon monoxide (CO) 200 to 300 times more than with oxygen, resulting in the formation of carboxyhemoglobin and preventing the binding of oxygen to hemoglobin due to the competition of the same binding sites.
Q. What is the difference between pulse oximetry and oxygen saturation?
Pulse oximetry is a way to measure how much oxygen your blood is carrying. The blood oxygen level measured with an oximeter is called your oxygen saturation level (abbreviated O2sat or SaO2). This is a percentage of how much oxygen your blood is carrying compared to the maximum it is capable of carrying.
Table of Contents
- Q. What is the difference between pulse oximetry and oxygen saturation?
- Q. How much o2 is bound to hemoglobin during rest?
- Q. Does co2 have a higher affinity for hemoglobin than O2?
- Q. How many co2 can hemoglobin bind?
- Q. Why does myoglobin have a high affinity for oxygen?
- Q. When will hemoglobin have the highest affinity for oxygen?
- Q. What causes the oxygen hemoglobin dissociation curve to shift to the right?
- Q. Which of the following will increase the affinity of hemoglobin for oxygen?
- Q. What is double Bohr effect?
- Q. What is the Bohr shift on the oxygen hemoglobin dissociation curve?
- Q. What is Bohr and Haldane effect?
- Q. What is meant by Bohr effect?
- Q. What is Bohr effect in respiration?
- Q. What causes the Haldane effect?
- Q. Which one of the following is applicable for Haldane effect?
- Q. How does Haemoglobin act as buffer?
- Q. What causes a leftward shift in the oxygen dissociation curve?
- Q. What does the term p50 indicate in reference to Oxy HB curves?
- Q. How does pH affect the oxygen dissociation curve?
- Q. What factors increase oxyhemoglobin dissociation?
- Q. Why is it hard for the first oxygen to bind to hemoglobin?
- Q. Why is hemoglobin curve sigmoidal?
- Q. Is hemoglobin hyperbolic or sigmoidal?
Q. How much o2 is bound to hemoglobin during rest?
Oxygen is carried in the blood in two forms: (1) dissolved in plasma and RBC water (about 2% of the total) and (2) reversibly bound to hemoglobin (about 98% of the total).
Q. Does co2 have a higher affinity for hemoglobin than O2?
Carbon monoxide has a greater affinity for hemoglobin than does oxygen. Therefore, when carbon monoxide is present, it binds to hemoglobin preferentially over oxygen. As a result, oxygen cannot bind to hemoglobin, so very little oxygen is transported throughout the body.
Q. How many co2 can hemoglobin bind?
four molecules
Q. Why does myoglobin have a high affinity for oxygen?
Myoglobin is a small oxygen-binding protein found in muscle cells. This allows the oxygen that is binded to have a negative charge, which stabilizes it. Myoglobin’s affinity for oxygen is higher than hemoglobin. And unlike hemoglobin which is found in the red blood cells, myoglobin is found in muscle tissues.
Q. When will hemoglobin have the highest affinity for oxygen?
Fetal hemoglobin has a higher oxygen-binding affinity than that of maternal hemoglobin. Fetal red blood cells have a higher affinity for oxygen than maternal red blood cells because fetal hemoglobin doesn’t bind 2,3-BPG as well as maternal hemoglobin does.
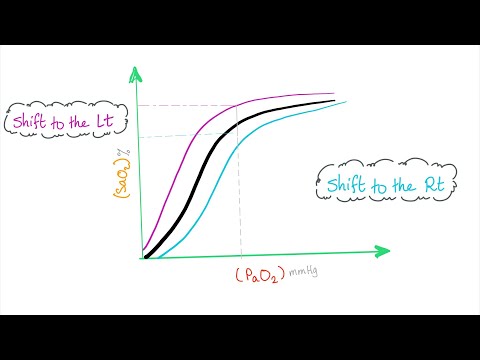
Q. What causes the oxygen hemoglobin dissociation curve to shift to the right?
The shift of the oxygen dissociation curve to the right occurs in response to an increase in the partial pressure of carbon dioxide (Pco2), a decrease in pH, or both, the last of which is known as the Bohr effect.
Q. Which of the following will increase the affinity of hemoglobin for oxygen?
Decreased carbon dioxide partial pressure will increase the affinity for oxygen rather than decrease it. Increased temperature and increased 2,3-bisphosphoglycerate will also decrease the hemoglobin affinity for oxygen.
Q. What is double Bohr effect?
The ‘double Bohr’ effect helps to increase fetal oxygenation. The transfer of carbon dioxide from fetal to maternal blood shifts the maternal oxyhaemoglobin curve to the right and the fetal curve to the left, facilitating the transfer of oxygen across the placenta from mother to fetus.
Q. What is the Bohr shift on the oxygen hemoglobin dissociation curve?
The Bohr effect is the shift to the right of the oxygen equilibrium curve of both adult and fetal blood in response to an increase in PCO2 or a decrease in pH, or both.
Q. What is Bohr and Haldane effect?
Haldane effect is what happens to pH and CO2 binding because of oxygen, and Bohr effect is what happens to oxygen binding because of CO2 and lower pH.
Q. What is meant by Bohr effect?
The Bohr effect describes hemoglobin’s lower affinity for oxygen secondary to increases in the partial pressure of carbon dioxide and/or decreased blood pH. This lower affinity, in turn, enhances the unloading of oxygen into tissues to meet the oxygen demand of the tissue.[1]
Q. What is Bohr effect in respiration?
The Bohr effect is a phenomenon first described in 1904 by the Danish physiologist Christian Bohr. That is, the Bohr effect refers to the shift in the oxygen dissociation curve caused by changes in the concentration of carbon dioxide or the pH of the environment.
Q. What causes the Haldane effect?
The Haldane effect is a property of hemoglobin first described by John Scott Haldane, within which oxygenation of blood in the lungs displaces carbon dioxide from hemoglobin, increasing the removal of carbon dioxide. Consequently, oxygenated blood has a reduced affinity for carbon dioxide.
Q. Which one of the following is applicable for Haldane effect?
The Haldane Effect describes the effect of oxygen on CO2 transport. The Haldane Effect (along with the Bohr Effect) facilitates the release of O2 at the tissues and the uptake of O2 at the lungs.
Q. How does Haemoglobin act as buffer?
As a buffer, hemoglobin counteracts any rise in blood pH by releasing H+ ions from a number of atomic sites throughout the molecule. Similarly, a number of H+ ions are bound to, or are ‘taken up’ by the molecule, acting to counteract a decrease in pH.
Q. What causes a leftward shift in the oxygen dissociation curve?
Carbon Monoxide The binding of one CO molecule to hemoglobin increases the affinity of the other binding spots for oxygen, leading to a left shift in the dissociation curve. This shift prevents oxygen unloading in peripheral tissue and therefore the oxygen concentration of the tissue is much lower than normal.
Q. What does the term p50 indicate in reference to Oxy HB curves?
p50 is the oxygen tension when hemoglobin is 50 % saturated with oxygen. When hemoglobin-oxygen affinity increases, the oxyhemoglobin dissociation curve shifts to the left and decreases p50. When hemoglobin-oxygen affinity decreases, the oxyhemoglobin dissociation curve shifts to the right and increases p50 (Figure 1).
Q. How does pH affect the oxygen dissociation curve?
In contrast, an elevated (= alkaline or basic) blood plasma pH of 7.6 causes the O2-Hb saturation curve to shift about 15% to the left of normal. As blood plasma pH decreases (= becomes more acidic), H+ ions increasingly bind to hemoglobin amino acids, which lessens hemoglobin’s affinity for O2.
Q. What factors increase oxyhemoglobin dissociation?
The oxygen–hemoglobin dissociation curve can be displaced such that the affinity for oxygen is altered. Factors that shift the curve include changes in carbon dioxide concentration, blood temperature, blood pH, and the concentration of 2,3-diphosphoglycerate (2,3-DPG).
Q. Why is it hard for the first oxygen to bind to hemoglobin?
It is easier to bind a second and third oxygen molecule to Hb than the first molecule. This is because the hemoglobin molecule changes its shape, or conformation, as oxygen binds. The fourth oxygen is then more difficult to bind.
Q. Why is hemoglobin curve sigmoidal?
Hemoglobin’s oxygen-binding curve forms in the shape of a sigmoidal curve. This is due to the cooperativity of the hemoglobin. Both these changes causes the hemoglobin to lose its affinity for oxygen, therefore making it drop the oxygen into the tissues.
Q. Is hemoglobin hyperbolic or sigmoidal?
THE CLASSICAL OXYGEN DISSOCIATION CURVE OF HEMOGLOBIN The shape of the oxygen dissociation curve of Hb is sigmoidal, whereas that of other oxygen-carrying molecules (such as Myoglobin) is hyperbolic.